
News about healthy eating is always easy to set off a circle of friends.
At the beginning of the 2018 New Year, a story about young women appearing [milk-colored] and [lard-colored] plasma and receiving ICU rescue appeared in major media.
In the title of the article, the [culprit] is all pointed at takeout.

Review of patient’s condition
Based on the reports of major media, we can roughly sort out such a case story:
The patient is a 27-year-old woman who has been healthy in the past and has an unhealthy diet lifestyle (likes to eat takeout food, is also a little fat, and does not like sports).
A week ago, abdominal pain occurred after meals, mainly in the right upper abdomen, accompanied by nausea and vomiting. At that time, I didn’t care.
After resting for two days, the patient’s abdominal pain did not improve significantly and dyspnea occurred. Therefore, he went to the local hospital for emergency treatment. CT scan showed pancreatic exudation. Admission diagnosis: acute pancreatitis.
After admission, the relevant examination was improved. It was obvious from the blood drawing that a layer of glistening oil was floating on the upper layer of the blood, and the blood pressure also exceeded the standard a lot (the doctor said in the news).
He was transferred to ICU (Intensive Care Unit) for plasma exchange therapy and urgent examination of blood lipid and other related indicators.
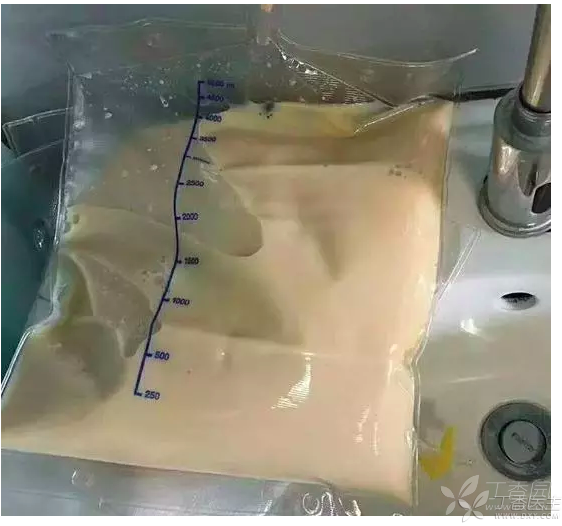
Return of blood lipid results: 30.01 mmol/L, while the normal standard is not higher than 1.7 mmol/L, and the normal upper limit of patients’ blood lipid exceeding the standard is nearly 18 times.
After 24 hours, bedside plasma exchange was performed again. After two exchanges, the patient’s symptoms improved significantly and his blood lipid gradually decreased. He was transferred back to the general ward on January 16.
Who is the real culprit?
In order to ensure the professionalism of the discussion, we invited professional station friends from Clove Garden to analyze this case:
1. Is the diagnosis and treatment of this case correct?
It is correct.
This patient is a typical hyperlipidemic pancreatitis. The patient was previously healthy (the previous blood lipid condition of the patient was not mentioned in the previous article), and transient abdominal pain aggravated with respiratory symptoms after diet.
Due to the pathophysiological characteristics of pancreatitis, a large amount of pancreatic lipase is secreted instantly, causing a sharp rise in plasma fat, and the rise of these blood lipid will bring accompanying symptoms.
Plasma exchange is an effective treatment method for it. Through plasma exchange, one’s own plasma is exchanged and new plasma is infused. On the one hand, blood lipid is reduced, and on the other hand, inflammatory factors in the body are reduced.
However, it cannot be said that the blood replaced is [milk blood] [lard blood]. Instead, it should be pointed out that the blood lipid rises sharply due to acute pancreatitis, and plasma exchange is the fastest way to treat this situation.
2. Will a high-fat diet definitely cause pancreatitis?
Not necessarily.
Although hyperlipidemia is a risk factor for pancreatitis, it is definitely not hyperlipidemia that leads to pancreatitis.
The main causes of pancreatitis are drinking and biliary obstruction (stones, roundworms, etc.). In addition, many factors such as trauma and pancreatic injury can also lead to pancreatitis.
In this case, the patient complained of abdominal pain after taking ice drinks after eating (take-out), but neither take-out foods nor drinks specified their specific ingredients, and the relationship between them and this acute pancreatitis could be confirmed.
3. Is this kind of situation common clinically?
It is quite common that the clinical laboratory can see such blood samples almost every day. Generally, the triglycerides of such blood samples far exceed normal values.
So why is there such blood? There are pathological reasons, 1. For example, the patient’s lipid metabolism disorder is itself hypertriglyceridemia 2. Chylous duct injury 3. Pancreatitis, etc.
There are physiological reasons, such as eating hot pot or mutton hotpot and other high-fat foods the day before, the blood will also appear the next day, this chylous blood is transient, the patient will recover quickly after a light diet.

4. If pancreatitis occurs, what kind of examination and treatment are needed?
Pancreatitis is a clinical multiple emergency, but it must not be underestimated.
Because pancreatitis, if delayed in treatment, can easily develop into severe pancreatitis and endanger life. Even if the rescue is successful, the residual infection and intestinal fistula in the later period will cause long-term pain to the patient.
How to correctly diagnose acute pancreatitis? Typical initial symptoms include sharp onset of upper abdominal pain, often accompanied by nausea, vomiting and radiation. Occasionally, subcutaneous skin ecchymosis (Gray-turner sign and Cullen sign) can be seen. It can be accompanied by one or more organ dysfunction and severe metabolic dysfunction.
The most timely imaging examination for the diagnosis of pancreatitis is abdominal enhanced CT. Hematuria amylase is an important auxiliary examination for the determination of pancreatitis. At the same time, bedside B-ultrasound examination can be performed at any time if the condition is complicated.
The treatment of hyperlipidemic acute pancreatitis also requires banning low molecular weight heparin and insulin, and adopting various methods (fat adsorption, plasma exchange) to rapidly reduce blood lipid.
Is what wrong with this news?
In this era of news explosion, how to identify unreliable news is actually a very interesting thing.
To sum up with the comments of a clove garden station friend:
My first reaction to the news was problematic.
Take-out = high-fat diet = hyperlipidemia = hyperlipidemia pancreatitis = plasma like milk and lard. This reasoning process is very lax.
Not to mention the conclusion that takeout leads to [lard] plasma.
The biggest problem in this news is not the case itself. In this case, the 27-year-old patient received timely treatment and finally recovered. This is a happy thing.
However, if we only publicize the harm of take-out food unilaterally, instead of clarifying the real problems of acute pancreatitis (drinking and stones), such publicity articles will bring negative effects. All these will become the pain of patients and the busyness of doctors.
The Chinese New Year is coming soon. At this time of year, there will be a large number of patients with acute pancreatitis.
They all took place at the New Year’s Eve dinner where the whole family gathered, drinking heavily and eating large pieces of meat.
