Spring is warm and cold at first, and the cold and hot weather really hurts parents.
Give the child more clothes, it’s too hot. Take off your clothes, it’s a little cold again.
After repeated tossing and turning, the child caught a cold and coughed without being careful.
Every cough, parents’ hearts also hang up, but don’t be pneumonia!
This kind of worry is not unreasonable. Many parents may find that when the child is only a small cold, how can it become more and more serious and even become pneumonia?
How to judge whether a child has a common cold or pneumonia? How to nurse children with pneumonia?
Does the child have pneumonia? Early judgment is very important.

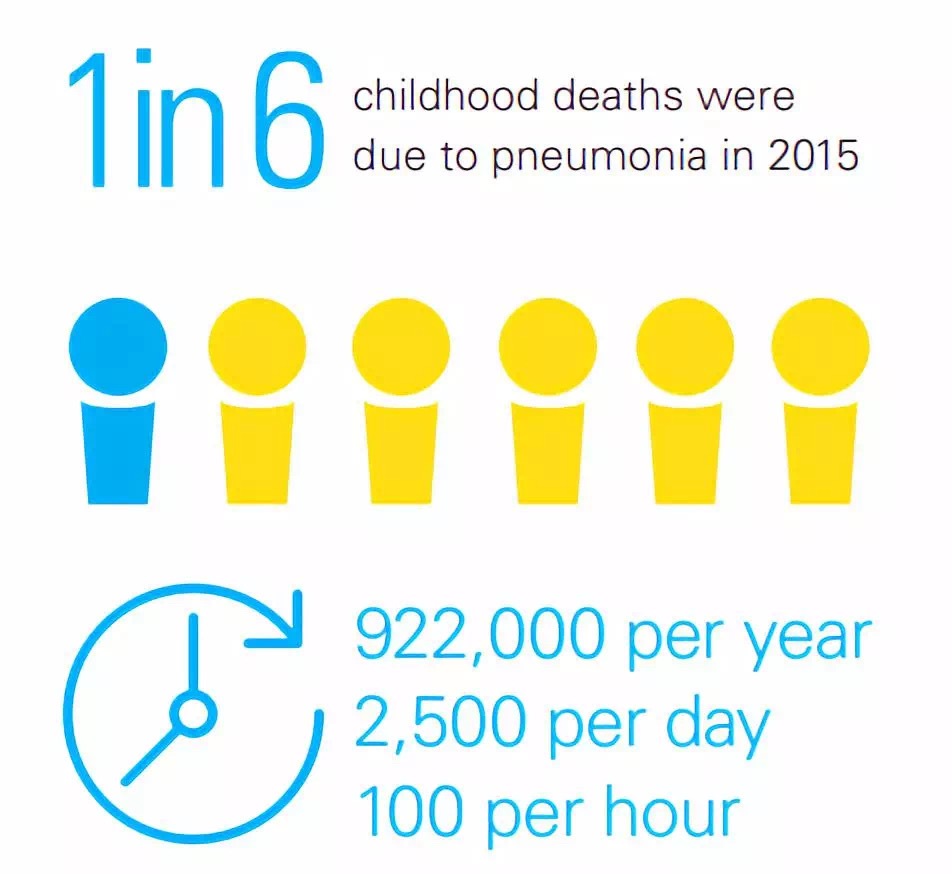
The reason why everyone is afraid of children getting pneumonia is mainly because pneumonia is too destructive.
It can cause children to cough, fever, chills, severe respiratory failure and death…….
According to estimates by the World Health Organization, pneumonia killed an estimated 925,000 children under the age of 5 in 2015. That is to say, 2,500 children died of pneumonia every day in 2015.
However, the early symptoms of pneumonia are usually similar to colds. Is there any what method that can be judged at the beginning of pneumonia so as to treat it early?
In fact, the identification of early pneumonia is also traceable.
1. Shortness of breath and accelerated respiratory frequency
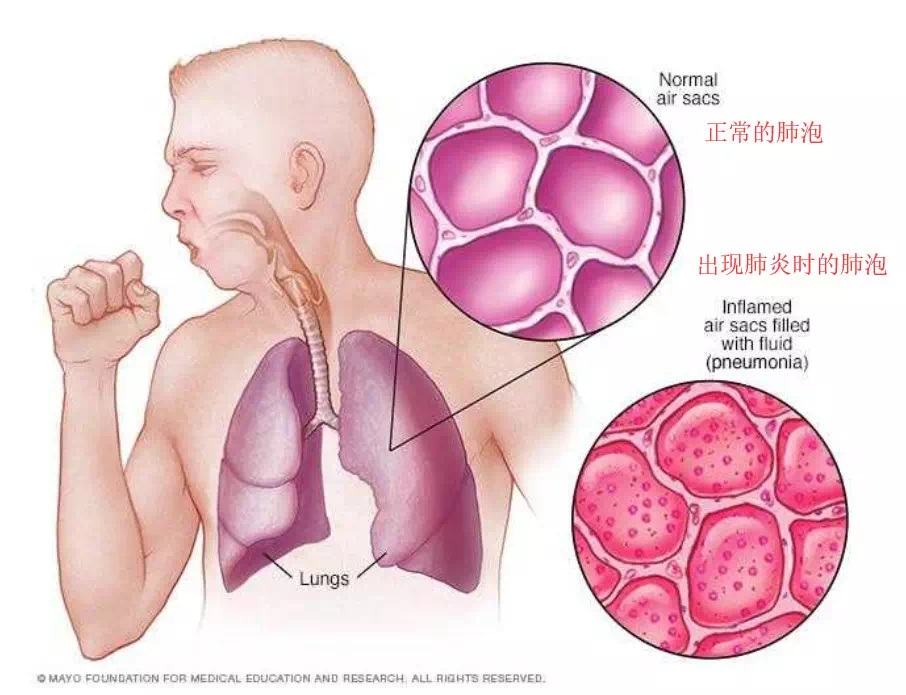
Pneumonia is caused by lung infection, which causes the alveoli originally filled with oxygen to be occupied by pus, oxygen is reduced, and gas exchange is difficult. Therefore, the most typical symptom of pneumonia is shortness of breath.
According to the WHO Plan for Prevention and Treatment of Acute Respiratory Infection in Children, the criteria for shortness of breath in children are:
· < 2 months old, breathing ≥ 60 times/minute;
2 ~ 12 months old, breathing ≥ 50 times/minute;
1 ~ 5 years old, breathing ≥ 40 times/minute;
· ≥ 5 years old: respiratory rate > 20 beats/minute.
How do you count?
1) Count when the child is quiet and fever subsides, because the child’s breathing frequency will vary with the activity.
2) Open the child’s clothes and count them by looking at the ups and downs of the chest. Auscultation may stimulate the child and lead to a pseudo-increase in respiratory frequency.
3) It is better to remember the complete 60 seconds for evaluation, with higher accuracy.
If the child’s breathing frequency exceeds the breathing frequency standard for the corresponding age, he should be alert to the possibility of pneumonia.
2. Severe fever and cough
The initial symptoms of a cold are usually manifested as nasal symptoms such as runny nose, sneezing, nasal obstruction, etc. The temperature of fever is around 38.5 ℃, rarely exceeding 39 ℃, and cough is mostly at night and in the morning, usually from the throat.
However, children with pneumonia may suffer from chills when they have a fever (manifested as fear of cold and shivering). When coughing, they sound deeper. When coughing, they turn red and even vomit, and the frequency is more frequent.
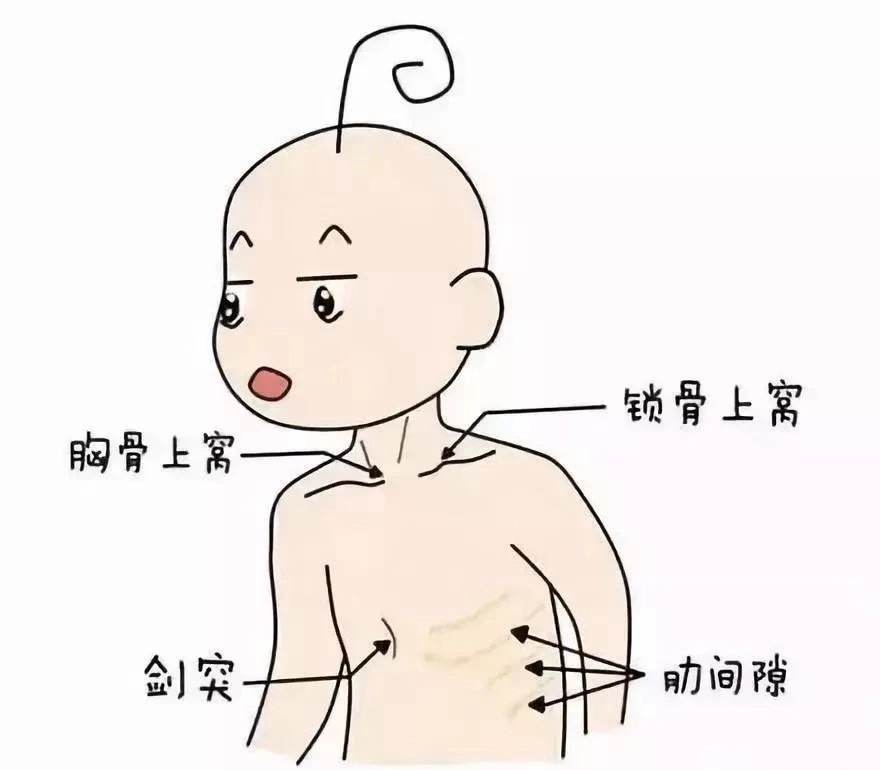
3. Triple concave sign is a sign of severe pneumonia.
It should be noted that if the child has three concave signs, it is likely to be severe pneumonia.
The so-called three concavity refers to the inward depression of the supracernal fossa, supraclavicular fossa and intercostal space during breathing.
Through the above three points, we can basically judge whether the child is pneumonia or the common cold.
However, not all children will have these three conditions when they get pneumonia. For example, newborns may not have typical symptoms of pneumonia such as fever and cough, but only manifested as faster breathing, choking on milk and bubbling in the mouth.
Many parents can’t distinguish pneumonia from common cold, which is actually closely related to the mechanism of pneumonia.
Whether a child will get pneumonia depends on whether the immune system can defeat the pathogen.

Pathogens enter through nasopharynx (upper respiratory tract) at first, and then go all the way down through trachea and bronchus. When infected with lungs (lower respiratory tract), pneumonia occurs.
If it is a common virus, the child’s own immune system is enough to eliminate him, and the child may only have some cold symptoms.
If it is a [high-level] pathogen such as influenza virus and adenovirus, the child’s immune system cannot resist it and the risk of contracting pneumonia will increase.
We cannot predict which virus invades the child’s body, nor can we predict whether the child’s immune system can defeat the pathogen, so we may miss the best treatment opportunity.
Fortunately, we can judge through the above three methods so that the child’s illness can be controlled as soon as possible.
If it is severe pneumonia, take medicine, take medicine, take injections.
If it is mild pneumonia caused by virus, it can be cared for at home under the guidance of doctors.
Nursing Pneumonia Children, Remember 5 Points

1. Proper use of antipyretics
Acetaminophen (Tylenol) can be used for more than 2 months and ibuprofen (Merrill Lynch) can be used for more than 6 months.
Step 2: Give sufficient liquid
Children who have added supplementary foods can be fed with water in small quantities and many times. Children who have not added supplementary foods for less than 6 months are not recommended to drink extra water and milk.
3. Give your child nutritious food
Children with pneumonia are usually in poor spirits and have poor appetite. Nutritious foods (meat, fish, eggs, etc.) help children restore energy and fight pathogens. Unless the child is allergic, there is no need to avoid eating.
4. Turn on the humidifier when the air conditioner is turned on at home or the air is dry.
When the air is dry, children are more likely to cough. Keeping indoor humidity at about 50% ~ 60% is helpful for the recovery of children’s illness. I don’t know how to deal with humidity. Just buy a hygrometer online.
5. Don’t smoke, don’t smoke, don’t smoke!
Children suffering from pneumonia are especially sensitive to pollutants in the air. Smoking at home will not only increase the risk of pneumonia, but also delay the recovery of the child’s illness.
Many parents will wonder: Why does a child become pneumonia when he is ill? Even sometimes, when the child has pneumonia, he thinks it is just a [severe cold].
In fact, these simple clinical standards can help parents to make an early identification of children’s pneumonia.
Pneumonia may be terrible, but what is more terrible is not preparing early.
Parents who master more judgment methods and know more prevention knowledge can make their children less dangerous.
